One theme I have noticed in admissions interview questions for medical school is that they want to see that applicants are well rounded, and do things other than study, work in a lab, or volunteer. I.e., that they involve themselves in activities that don’t necessarily strengthen their med school applications. That they know how to decompress and relax. Because these are skills that are so important, especially in such a high-pressure field. So, one of the ADCOM questions I want to answer is this: Discuss a book that you have recently read for pleasure. Why does this book interest you?
And here was my answer, as of a few days ago: Uhhhh … pleasure? I don’t have TIME to read for pleasure!
Thankfully, I do have a little more time now, as I am not in school (and inundated with the requirement of reading textbooks). So I picked up a of book a few days ago, and started reading for “pleasure” again. And it’s felt absolutely wonderful. While I haven’t finished it, I will tell you a little bit about it, and what I have learned thus far. I will also share my reading list, books that I hope to read throughout the next months (when I will still have more time, before the insanity of medical school starts).
What I’m Currently Reading:
 Nature’s Robots: A History of Proteins
Nature’s Robots: A History of Proteins
(Charles Tanford and Jacqueline Reynolds, 2004)
I downloaded this Kindle book (to read on my iPad) on Dec. 25, 2011, according to my Amazon.com account. And honestly, I totally forgot I had it. But I was looking at my Kindle books a few days ago, and there it was! I was thrilled, it was like Christmas (even though I bought it for myself). I started reading it that evening. And was pleasantly surprised. It’s definitely a history book, at least thus far. But there’s a lot of science – especially chemistry and biochemistry – in there, which makes me happy. And the authors detail a lot of the theories, and arguments over theories, that were proposed in the past regarding proteins. I’ve made it through chapter 5, and am quite pleased with how the book is going. Proteins were my first “love” in science, and they continue to fascinate me. They are such an important part of our lives, and anyone who is in the biological sciences needs to have a good understanding of them. Learning about their history, in terms of scientific advances, is a way for me to understand where we have been, as a scientific community, and also to be inspired about where we are going in the future.
My Future Reading List:
Fiction:
 The Life All Around Me by Ellen Foster
The Life All Around Me by Ellen Foster
(Kaye Gibbons, 2011)
One of my favorite authors is Flannery O’Connor, and Kaye Gibbons reminds me of O’Connor (very high praise, in my book – pun intended). This book is a follow-up to the book Ellen Foster, which I read several years ago. After reading that, I flew through several other Gibbons novels. I look forward to reading more about this lonely girl, and the struggles she goes through.
 A Wizard of Earthsea
A Wizard of Earthsea
(Ursula Le Guin, 1970)
I was first exposed to Ursula Le Guin when I was a textbook editor, and worked on the American Literature lesson for the hilarious but disturbing short story SQ. “SQ” stands for “sanity quotient,” and the story is a wonderful parody. I highly recommend it, even if you are not a huge short story lover (I am not). I immediately checked out Le Guin’s Earthsea series, and this book is the first of that series. I have read it before, but I want to read it again. And I rarely read books twice, simply because there are so many books I want to sample.
On your Facebook info page, you can list favorite quotations. I have only one listed, and it’s from this book, from the creation story that is entwined throughout. I find it beautiful, poignant, and enigmatic, something to ponder:
Only in silence the word,
only in dark the light,
only in dying life:
bright the hawk’s flight
on the empty sky.
– The Creation of Éa
Memoirs:
 Genetic Rounds: A Doctor’s Encounters in the Field That Revolutionized Medicine
Genetic Rounds: A Doctor’s Encounters in the Field That Revolutionized Medicine
(Robert Marion, 2009)
This book, which I found rather randomly while searching my library’s online catalog, looks fascinating to me. I don’t know much about it, don’t know whether it’s well written, but the topic is definitely something that interests me. I enjoy a good medical memoir for sure, because it gives me a glimpse into the field I will be entering soon. And this one piqued my curiosity in particular because it marries medicine and genetics, which is something I am interested in doing myself in the future.
 The Spirit Catches You and You Fall Down
The Spirit Catches You and You Fall Down
(Anne Fadiman, 2012)
This was recommended to me by a physician I highly respect as “must read” for any physician, or physician-to-be. According to Amazon, its “explores the clash between a small county hospital in California and a refugee family from Laos over the care of Lia Lee, a Hmong child diagnosed with severe epilepsy. Lia’s parents and her doctors both wanted what was best for Lia, but the lack of understanding between them led to tragedy.” Given my interest in multicultural issues, and health literacy, it seems a poignant book to read right now.
Nonfiction:
 The Immortal Life of Henrietta Lacks
The Immortal Life of Henrietta Lacks
(Rebecca Skloot, 2011)
One of my dear friends – who is most definitely not a science person – read this book and told me it was amazing. Here is a portion of the summary posted on Amazon: “Her name was Henrietta Lacks, but scientists know her as HeLa. She was a poor Southern tobacco farmer who worked the same land as her slave ancestors, yet her cells—taken without her knowledge—became one of the most important tools in medicine. The first “immortal” human cells grown in culture, they are still alive today, though she has been dead for more than sixty years. If you could pile all HeLa cells ever grown onto a scale, they’d weigh more than 50 million metric tons—as much as a hundred Empire State Buildings. HeLa cells were vital for developing the polio vaccine; uncovered secrets of cancer, viruses, and the atom bomb’s effects; helped lead to important advances like in vitro fertilization, cloning, and gene mapping; and have been bought and sold by the billions.”
If you read any scientific literature, you are bound to come across HeLa cells as a subject of study. Reading the story of their “birth,” so to speak, and such a controversial and heartbreaking one, seems like a natural thing to do for a budding scientist such as myself.
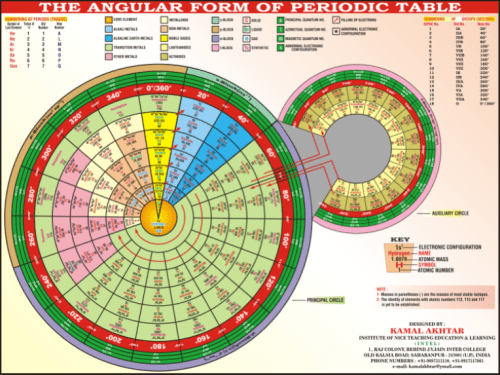
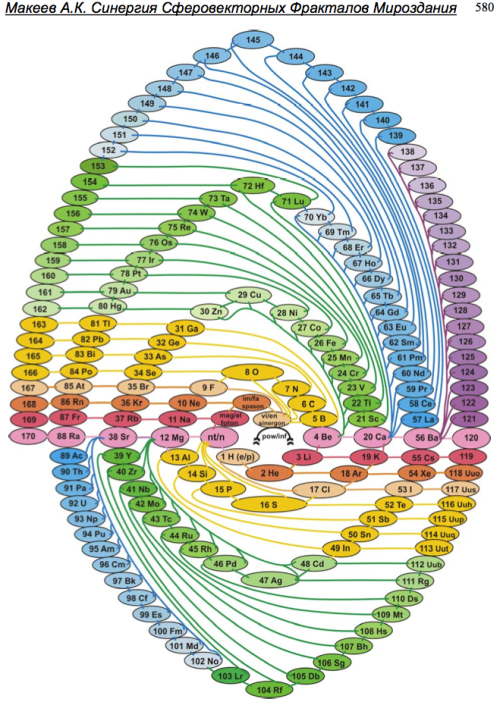
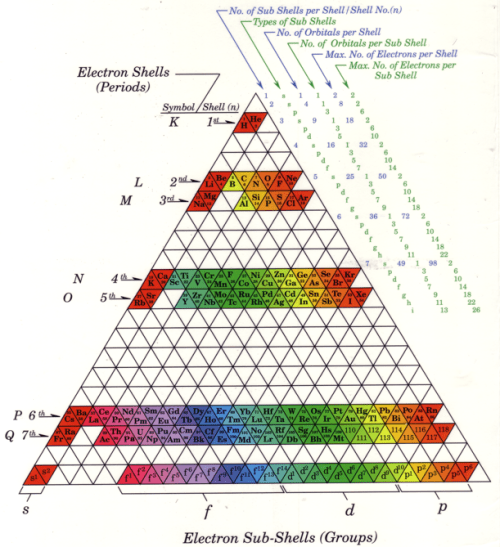
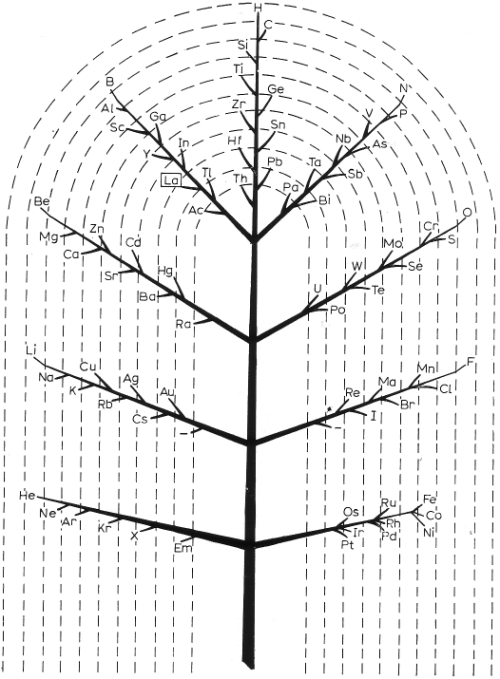
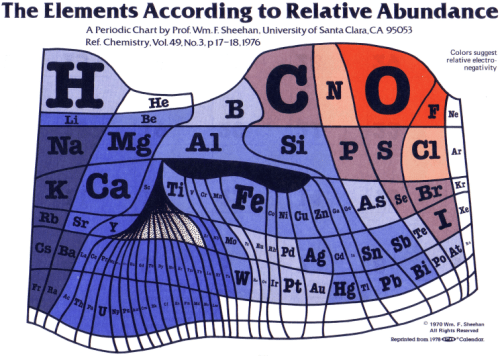
 The Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the Elements
The Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the Elements
(Sam Kean, 2011)
It was my chemistry major friend who recommended this one to me. And as you know from some of my previous posts, chemistry – and the periodic table – have piqued my interest of late. I look forward to reading the history of this seminal scientific tool. This is what the Amazon summary says about the book: “The Periodic Table is a crowning scientific achievement, but it’s also a treasure trove of adventure, betrayal, and obsession. These fascinating tales follow every element on the table as they play out their parts in human history, and in the lives of the (frequently) mad scientists who discovered them. THE DISAPPEARING SPOON masterfully fuses science with the classic lore of invention, investigation, and discovery–from the Big Bang through the end of time.” Sounds pretty cool, eh?
Conclusion:
Clearly, I have plenty to keep myself busy. The wonderful thing is, I’m not afraid to use my local library (or the wonderful library loan system). So reading all of these amazing books won’t cost me anything. In addition, a couple of these books are available through my library’s digital lending center, which will allow me to read them on my iPad. As I read these treasures, I will definitely post about them. So stay tuned …