Back to Uganda …
by Lorien E. Menhennett

In less than 2 weeks, I’m headed back to Uganda for another palliative care research project. This picture was taken during my first trip there in July of 2016.
I’ve mentioned in several recent posts that I’m on a four-month research rotation. Then I realized that I haven’t said anything about what I’m actually doing. It’s time to change that.
Before I delve into the details of the project itself, though, I need to provide some background and context so that the project itself makes sense.
Those of you who have been following along for a while may remember that I went to rural Uganda in July of 2016, the summer after my first year in medical school. I went with a palliative care physician from Cornell, Dr. Randi Diamond, to do both clinical and research work, looking (in part) at the understanding palliative care patients there have of their illnesses, and why people present at such late stages of illness to the medical system.
One thing palliative care patients told us during that trip was that they perceived their health care workers to have poor communication skills. And as a result, the patients were distrustful of medical workers, and the health care system as a whole.
In rural Uganda, it’s also important to know that medical workers have limited access to continuing medical education (“CME”). Much of the palliative care CME (and CME in general, for that matter) is Internet-based. As I learned during my first trip there, even in places that have the equipment for Internet, it’s completely unreliable. Not only that, but medical education materials are mostly developed for a Western audience like ours — one with incredible resources. What’s discussed and taught isn’t always relevant to medical workers in rural Africa, who work in a very different environment, as you can see from pictures I’ve included below, taken during my first trip there. (If you want to read in more detail about the hospital environment in Uganda, here is a post I wrote about it in 2016.)
All of this got Dr. Diamond and me thinking about whether we could do something to help improve communication skills among health care workers in rural Uganda.
As did some things we learned from an organization we’ve now partnered with on this new project, the African Palliative Care Organization (APCA). APCA has developed its own palliative care curriculum for use in Africa, and one of the key competencies is communication. In developing this curriculum, they did a needs assessment, and found “communication” to be one of the gaps in both skills and knowledge in health care workers there. They also found a shortage of culturally appropriate materials for teaching palliative care.
Putting all this together, there is a clear need for culturally appropriate continuing education directed at communication skills.
Both Dr. Diamond and I found ourselves in a unique place to help fill that need. During Dr. Diamond’s last two summer trips to rural Uganda (2016 and 2017), a documentary film crew accompanied her and the local Ugandan palliative care outreach team on home visits to palliative care patients. So she has footage of palliative care taking place in rural Uganda, with local medical workers, that could be used to illustrate best practices.
As part of Cornell’s curriculum, I have 6 months to do full-time research, 4 months now and 2 months at the beginning of 2019. After my first trip to Uganda in 2016, I knew I wanted to work with Dr. Diamond again, and go back to Uganda. From my past life as a textbook editor and freelance writer, I also have experience in developing educational materials.
It was a perfect match.
In less than 2 weeks, we leave for Uganda to pilot test the multimedia educational modules we have developed. There are 3 different modules:
- Basic Communication Skills in Palliative Care
- Delivering Bad News
- Pain Assessment (with a focus on the communication aspect of assessing pain)
Each module includes the video clips I mentioned, and a teaching guide that Dr. Diamond and I wrote. The teaching guides have educational content as well as reflection questions to get people thinking about how what they’re learning applies to their own lives, and their own patients. This kind of “reflective practice” is so important in palliative care (and all of medicine, really). It’s not done much in Uganda, but it’s something that APCA has identified as a goal for integration into medical education there.
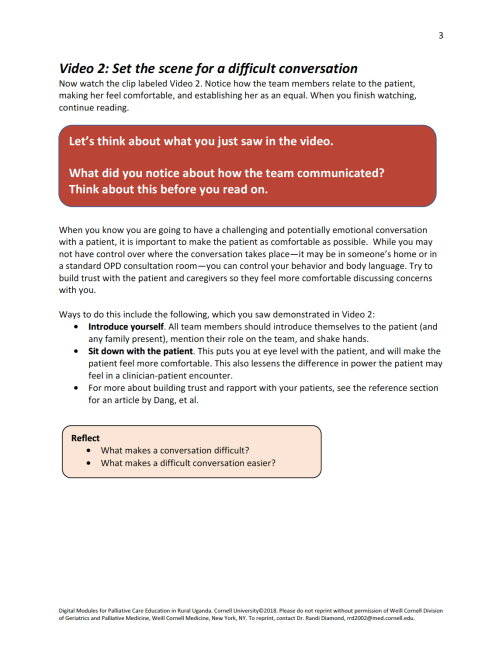
To give you an idea of what we’ve created, here is a page from the “Basic Communication Skills in Palliative Care” module:
Here are the basics of our research design:
Hypothesis: Communication training with culturally appropriate modules will enhance health worker confidence in, and knowledge base about, communicating with PC patients.
Methods:
- Pilot test the modules at 6 different rural sites in Uganda, identified by APCA
- Hoping for 6-12 participants per site (targeting medical workers such as physicians, nurses, and nurse assistants who interact with palliative care patients)
- Planning to test 2 of our modules at each site
- Conduct pre- and post-intervention surveys to assess the effectiveness of the modules
- Surveys will assess both knowledge base about, and confidence in, palliative care topics and skills
- Future data analysis will measure whether there is a change in knowledge and/or confidence after the participants complete the module
This project is not just about research, though. It’s also about leaving something behind that people can actually use. At the conclusion of each pilot testing session, we will leave printed copies of our teaching guides, as well as flash drives with the video clips and the teaching guides in PDF form. Hopefully, this strategy resolves the access issue; while Internet is spotty, these rural sites do have computers.
I’m in full trip-prep mode right now: assembling the printed guides, survey packets, mosquito repellent, and lots of protein to take with me for the month I’ll be there (the Ugandan diet is mostly starch based).
I’ll be based at the same place where I stayed during my last trip, St. Francis Naggalama Hospital, working with the wonderful Naggalama Hospital Palliative Care Outreach Team. I will sometimes have Internet access there (hopefully, more often than not). As I do, I will try to post updates on my trip.





What a win-win-win… situation! You’re making a difference in palliative care in Uganda, having an effect on patients and families lives, and getting to do some research using your gifts and past experience, plus traveling across the world! 🙂
LikeLike
Yes! 🙂
LikeLike
[…] box of notebooks. I mentioned in my last post that in our teaching guides, we include reflection questions to try to get people thinking about […]
LikeLike
Hi! OmG, how serendipitous for me to discover your blog. Incidentally, I am from Uganda originally, and I’ve lived in the states for the past 13 years. **And,** I am also transitioning into medicine from a different profession, i.e. academia. Thanks for this post, and best of luck in the rest of your med-school program and medical career.
–Seif S.
LikeLike
Wow, how serendipitous indeed! Thanks for your kind words. Best wishes to you, too, as you pursue medicine. If you have any questions about medicine as a second career, feel free to contact me. There’s a “contact” button on the top of my blog page. Take care!
LikeLike